Benign Paroxysmal Positional Vertigo
INTRODUCTION:
Benign Paroxysmal Positional Vertigo (BPPV) is a common type of dizziness caused by debris that has collected in the semicircular canals of the inner ear and that interferes with their normal function. This disorder increases in incidence with age, but may be seen in persons of any age. In persons over the age of 50, about half of all dizziness symptoms are attributable to BPPV. In general, about 20% of dizziness is caused by BPPV and 9% of all older persons have BPPV.
SYMPTOMS:
The symptoms of BPPV include vertigo, light-headedness, disorientation, disequilibrium, imbalance and nausea. The most characteristic symptom of BPPV is a violent spinning which lasts for only 5 to 15 seconds. Activities which bring on symptoms will vary in each person but always involve movement or position changes of the head or body. A patient may be sensitive to certain position changes for days, weeks, or months. The strength of the symptoms tends to diminish before they disappear. Approximately 30% of patients experience recurrences of BPPV symptoms. The most characteristic provocative motions include rolling over in bed and tipping the head back to back to look up. Typical histories include severe bursts of vertigo which begin while using a hair dryer, when having hair washed in a beauty parlor, removing items from a top kitchen shelf or when looking up to change a ceiling-mounted light bulb. More constant non-episodic symptoms, such as chronic lightheadedness or disequilibrium are also common, especially in individuals who carefully avoid all provocative movements and positions.
CAUSES:
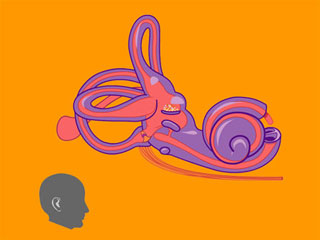
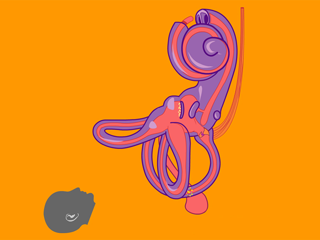
BPPV is caused by a displacement of tiny calcium carbonate crystals called otoconia (ear stones) from the utricle (a balance organ in the inner ear) into the semicircular canals, where they remain trapped and interfere with the normal function of the balance canals. After otoconia are loosened, they are normally absorbed by special cells (dark cells) around the utricle where they arise. If too many otoconia fall off at once, they may find their way into the semicircular canals before they can be absorbed. This typically occurs while the patient is lying down. The trapped particles continue to move within the semicircular canals after the head changes position, and cause the canals to send the brain inaccurate signals that the head is still moving. The result is bursts of severe vertigo brought on by changes in head position.
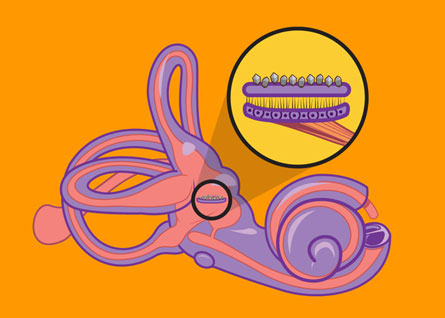
Otoconia on Utricle
For BPPV to occur, otoconia have to be displaced from the utricle into the semicircular canals. More otoconia tend to fall off of the utricle as we age and off of a utricle which has been injured by a virus or migraine. BPPV is 3 times more common among patients with migraine. Otoconia are commonly shaken from the utricles in head trauma and even in high-impact fitness activities.
The most common form of BPPV comes from debris trapped in the posterior semicircular canal. This is the form illustrated above and in the animation below. Approximately 5% of patients may also have symptoms of BPPV from debris trapped in the horizontal semicircular canal. Even fewer patients have debris trapped in the superior semicircular canal. Most commonly, the horizontal or superior canals are affected in addition to the posterior canal.
Because BPPV is more likely to occur in a sick ear which may be causing symptoms of dizziness, the straightforward positioning symptoms of BPPV may not be easily recognized. Similarly, BPPV may continue to recur if the underlying trauma (e.g. migraine, high-impact exercise) is not recognized and treated or prevented. In cases with atypical findings and in which multiple balance system pathologies co-exist, a full diagnostic work up may be required in order to distinguish pathologies which will require different forms of therapy.
OTOCONIA ON UTRICLE
Otoconia in canal
DIAGNOSIS:
The diagnosis of BPPV is relatively straight-forward due to the characteristic history and rotary vertigo which can be induced using the Hallpike maneuver. In this maneuver, the patient sits up on the exam table, turns the head 45° to one side, and lies down flat. It is repeated on each side. If a significant number of displaced crystals are present in the semicircular canals on the side to which the head is turned, vertigo will be provoked. The symptoms typically begin a few seconds after the lying down position is reached and last for about 5-15 seconds. The physican can determine the canal or canals involved by analyzing the eye movements provoked. Vertigo can also be provoked after the patient arises from the lying down position.
TREATMENT:
BPPV usually goes away by itself within six months of onset because of changes which occur both within the semicircular canals and in the brain. These processes cannot take place if the central nervous system has lost its ability to adapt to chronic abnormal stimulations, if the patient carefully avoids positions which provoke the vertigo, or if the ear continues to be injured by processes such as aging, migraine, or trauma. Such patients may have symptoms for years before presenting to the clinic. Vestibular suppressant medications are rarely effective because the characteristic symptoms are so violent and brief.
The treatment of this common vestibular disorder involves head movements designed to either 1) displace the otoconia from the affected semicircular canal(s) back into portion of the inner ear where there is an active mechanism for their resorption or 2) move the otoconia back and forth within the canal to promote their dissolution. Physical maneuvers to displace otoconia from the affected semicircular canal differ according to the canal affected.
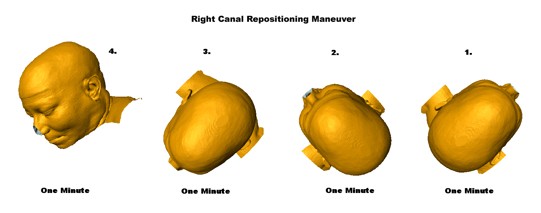
The canalith repositioning procedure (CRP) is a series of head maneuvers which displaces debris collected within the posterior semicircular canal out of the canal back into the utricle where they can cause few symptoms. This maneuver is successful in approximately 85% to 90% of cases and is usually performed in the office by a clinician with special expertise in balance disorders. To be effective, the clinician must correctly determine which ear is affected. Patients who choose to have this done must be willing to sleep semi-recumbent or vertically the night after the maneuver is performed. In patients with chronic, recurrent BPPV, the canalith repositioning procedure can safely be done at home, following specific instructions given by their clinician. As seen in the figures below, the CRP sequence differs for left and right posterior canal BPPV. We have found that the performance of a single daily CRP before arising from bed in the morning is an effective and efficient way to prevent symptoms in patients with chronic recurrent BPPV. In some severe cases, we have had success teaching patients to perform a home CRP for the right and left ears on alternating days.
- Download instruction sheet for daily home CRP for the right ear
- Download instruction sheet for daily home CRP for the left ear
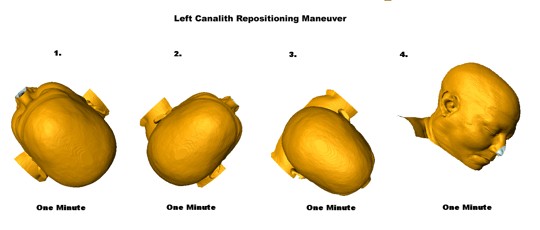
Watch Dr. Teixido demonstrate the canalith repositioning maneuver for the left ear
Watch Dr. Teixido demonstrate the canalith repositioning maneuver for the right ear
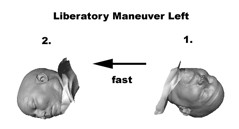
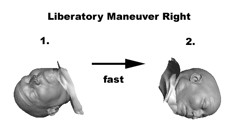
The Semont liberatory maneuver moves otoconia around the circumference of the posterior semicircular canal in fewer steps than the CRP. In this maneuver, a rapid change in head position moves the otoconia from the posterior semicircular canal back to the utricle before they start to fall back into the posterior canal. Afterwards, when the patient sits upright, the otoconia move to the utricle, where dark cells may facilitate resorption of otoconia. To be effective, an extreme head tilt in the first position, and a rapid transition to the second position are necessary. This may be difficult to do in many patients who have limited mobility.
Watch Dr. Teixido demonstrate the liberatory maneuver for the left ear
Watch Dr. Teixido demonstrate the liberatory maneuver for the right ear
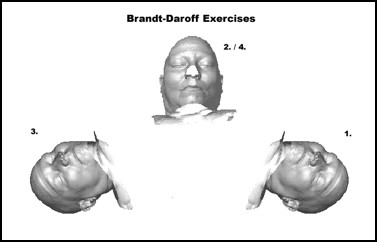
Brandt-Daroff exercises can be performed by the patient at home after they have been well-instructed in the physician’s office. These exercises may help to dissolve otoconia trapped within the semicircular canal. They are successful in over 90% of cases but must be performed properly and regularly. In most persons, complete relief of symptoms is obtained by one week. Once learned, these exercises are safe and effective for patients to repeat at home in the event their symptoms recur.
Download an instruction sheet for Brandt-Daroff exercises
Watch Dr. Teixido demonstrate Brandt-Daroff exercises
Posterior canal exercises are a modification of the Brandt-Daroff exercises. This treatment modification for posterior canal BPPV was developed in August 2006 by Dr. Teixido in the 3D visualization laboratory at the Delaware Biotechnology Institute. This exercise is appropriate for any BPPV patient, even if the side of disease is not known. The posterior canal exercise moves otoconia 60° farther around the circumference of the posterior semicircular duct with each repetition than conventional Brandt-Daroff exercises. The extra motion toward the posterior canal ampulla may enhance contact of the otoconia with cells at the base of the ampulla which may play an important role in otoconia resorption. The effectiveness of these new exercises is currently being studied in a single-blinded clinical trial.
Download an instruction sheet for posterior canal exercises

Watch Dr. Teixido demonstrate Posterior Canal Exercises
Surgery for BPPV may be performed if these conservative courses of treatment are ineffective in controlling symptoms. The surgery involves opening the inner ear and blocking the lumen of the posterior semicircular canal. This prevents otoliths which accumulate in the canal from affecting the sensitive balance trigger at its base. This procedure is highly effective, but there is a small risk to hearing.
Download a presentation on the biomechanics of BPPV (PDF)
WHERE CAN I LEARN MORE ABOUT BPPV?
BIBLIOGRAPHY
- Epley JM. The Canalith Repositioning Procedure for Benign Paroxysmal Positional Vertigo. Otolaryngology Head and Neck Surgery 1992; Volume 107; 399-404.
- McClure J. Horizontal Canal BPV. Journal of Otolaryngology 1985; 14:30-5.
- Baloh RW, et. al. Horizontal Semi-Circular Canal Variant of Benign Positional Vertigo. Neurology 1993; 43:2542-9.
- Cams LS; McClure JA Posterior Semi-Circular Canal Occlusion With a Normal Hearing Ear. Otolaryngology Head and Neck Surgery 1991; 104: 52-7.
- Semont A, et. al. Curing of the BPPV with a Liberatory Maneuver. Advances in Otorhinolaryngology. 1988; 42: 290-3. .
- Brandt T, Vertigo: its multisensory syndromes. 1991, London: Springer-Verlag.
- Oghalai JS, et al., Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg, 2000. 122(5): p. 630-4.
- Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol 1980. 106(8):484-485.
- Bertholon P, Chelikh L, Tringali S, Timoshenko A, et al. Combined horizontal and posterior canal benign paroxysmal positional vertigo in three patients with head trauma. Ann Otol Rhinol Laryngol 2005. 114:105-10.
- Cohen HS et al. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Arch OHNS 1999. 132(5): 501-505.
- Cohen HS et al. Treatment variations on the Epley maneuver for benign paroxysmal positional vertigo. Am J Otolaryngol 2004. 25(1):33-37.
- Fife TD. Recognition and management of horizontal canal benign positional vertigo. Am J Otol 1998. 19(3):345-351.
- Hain TC, Helminski JO, Reis I, Uddin M. Vibration does not improve results of the canalith repositioning maneuver. Arch Oto HNS 2000. 126:617-622.
- Hain TC, Squires TM, Stone HA. Clinical implications of a mathematical model of benign paroxysmal positional vertigo. Ann NY Acad Sci 2005. 1039:384-94.
- Moriarty B et al. The incidence and distribution of copular deposits in the labyrinth. Laryngoscope 1992. 102(1):56-9.
- Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol 1990. 99(5 Pt 1):330-334.
Information Provided by Dr. Michael Teixido, MD
Dr. Teixido is a board certified Otolaryngologist and Otologist/Neurotologist, with a special interest in medical and surgical conditions that affect hearing and balance. He is actively pursuing his goals of advancing the study and understanding of problems involving hearing and balance as a result of hereditary hearing conditions in his own family. View Dr. Teixido's Full Bio
FOULKSTONE
PLAZA
1401 Foulk Road.,
Suite 205
Wilmington, DE 19803
Phone: (302) 998-0300
Fax: (302) 478-8069
Greenville
Location
1011 Centre Rd,
Suite 200,
Wilmington DE 19805
Phone: (302) 998-0300
Fax: (302) 543-8456
MIDDLETOWN
CROSSING
306 EastMain Street
Middletown, DE 19709
Phone: (302) 998-0300
Fax: (302) 376-5251
NEWARK- IRON HILL
CORPORATE CENTER
700 Prides Crossing
Suite 200
Newark, DE 19713
Phone: (302) 998-0300
Fax: (302) 998-5111
